Drug Development Pathway for New & Generic Narrow Therapeutic Index Drugs

Drug development is a complex and intricate process that involves a significant amount of time, effort, and resources. One area of drug development that requires particular attention is the development of Narrow Therapeutic Index Drugs (NTIDs). These medications have a narrow range between the dose required for clinical effectiveness and the dose that causes significant adverse effects or toxicity, making them particularly challenging to develop and manage.
In this blog, we will explore the drug development pathway for new and generic NTIDs, including the importance of risk management, bioavailability, bioequivalence, and the management of risks and benefits. We will also discuss the challenges associated with developing and managing NTIDs and explore potential solutions and strategies for overcoming these challenges.
Narrow Therapeutic Index Drugs (NTIDs)
A narrow therapeutic index (NTI) drug is a medication for which the therapeutic range between the dose required for clinical effectiveness and the dose that causes significant adverse effects or toxicity is very small. In other words, a small difference in dose or blood concentration can change an effective treatment to serious therapeutic failures and/or life-threatening adverse drug reactions, and persistent disability.
Because of the narrow therapeutic range of these medications, there is a higher risk of side effects or toxicity careful monitoring and dose adjustments are required For this reason, the FDA and other regulatory agencies often require additional bioanalytical testing and monitoring for NTI drugs to ensure their safety and efficacy.
Healthcare providers must be highly skilled in dosing and monitoring Narrow Therapeutic Index Drugs, and they must be able to quickly recognize and manage adverse reactions. This additional testing also applied to the generic products of this NTID compound, which they required to pass the stricter bioequivalence criteria as defined by agencies.
Although the significant importance of NTID is nondebatable, and the general definition is well agreed upon by authorities, researchers, and physicians, no criteria for NTID classification has been established, neither has an approved list of NTIDs. Therefore, some drugs, such as warfarin, tacrolimus, or cyclosporine, are well-known as Narrow Therapeutic Index Drugs based on the authorities’ guidelines (e.g., FDA/EMA product-specific guidance), literature articles, and all other scientific discussion formats. While other drugs are under discussion on whether it belongs to this class.
Amifampridine for example, was reported in the literature to have a narrow therapeutic index and its exposure is associated with an increased risk for epileptic seizures. Titration from the lowest dose to a therapeutic effective dose is required for all patients. However, the FDA product-specific guidance for this compound requires the regular average bioequivalence approach, implying this drug is classified as a non-narrow therapeutic index drug per FDA reviewers. The pooled safety data from clinical trials reported seizures occurred for a dose equal to 40 mg and above. This was dose-dependence, and not all events required drug discontinuation or reduction.
Therefore, it’s important to differentiate a drug with a small therapeutic index or high-risk safety profile, from an NTID that a small change in dose or concentration is the consequence to threaten the patient’s safety or the drug’s effectiveness. Moreover, since there are no standard criteria to define, the sponsor should review the correlations between safety and pharmacokinetics, and between pharmacokinetics and pharmacodynamics to determine if additional measurements should be added to the drug development plan and the target clinical indication.
Risk Management for Narrow Therapeutic Index Drugs
“Risk management” or “Risk/benefit ratio” is one of the most popular terms for all pharmaceutical developers. To be approved for marketing, all new drugs must be able to demonstrate that their benefits outweigh the risks. This also applied to the clinician when choosing the treatment.
-
- How safe and effective is the drug?
- What is the disease being treated?
- What is the duration of treatment?
- What is the degree or severity of adverse events?
- What is the duration of adverse events?
Those questions are especially relevant for Narrow Therapeutic Index Drugs. Successfully supporting the risk management for an NTID is often more challenging due to the steep dose-response relationship and the small degree of separation between the two dose-therapeutic effects and dose-toxicity effects.
The situation can be more complicated when the drug has multiple serious adverse events and/or indications. Multiple formulations with various release profiles also complicate drug development. Therefore, Narrow Therapeutic Index Drugs might require more clinical trials to evaluate the different release profiles, indications, toxicity, and their correlations.
Additionally, a compound can be considered to have non-NTI for one indication but to have NTI for another indication. Aspirin is well-known as an Over-the-counter drug with a very wide range of antiplatelet and painkiller indications. However, when being prescribed for rheumatoid arthritis, the required aspirin dose is up to 4-6 g per day, which is close to the dose that results in undesirable toxicity. At this therapeutic range, aspirin demonstrated the characteristic of an NTID in which the therapeutic effect curve is very close to the toxicity effect curve.
The example also suggested besides evaluating the safety and effectiveness profiles, establishing dose regimens including titration up-down, the start and maintenance dose in parallel with introducing a quantifiable measurement for monitoring dose/blood concentration with safety and therapeutic effects are also essential for a Narrow Therapeutic Index Drug development plan. The clinical trials must identify one or several reliable tools that are not only scientifically but practically appropriate for clinical settings on the target patient population.
The ideal tools should include at least one non-subjective, non-bias measurement, which can be correlated with the physical/mental symptoms observed in patients. For instance, warfarin titration is based on the International Normalised Ratio (INR) result, which is a simple blood test that does not require any preparation and can be provided at a local clinic and/or at home at per patient’s convenience. The INR directly This is also a routine test required for patients with a high risk of thromboembolic events even if they are on another treatment than warfarin, thus, making it a useful and convenient tool for this NTID monitoring.
In a veritable manner, although there is a certain guide on which aspect should be evaluated for a new drug, there is no same old path for all. Each drug, depending on its characteristic, might require more or fewer studies to sufficiently support its risk/benefit profile.
Bioequivalence for Narrow Therapeutic Index Drugs
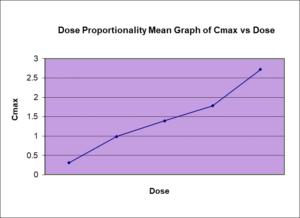
In contrast with a new drug application, the bioequivalence assessment for a generic NTID product is more established with tighter standards for the manufacture, in vitro, and in vivo assessments. Similar to the regular bioequivalence criteria, the criteria for NTID are also based on the key pharmacokinetic (PK) parameters for the rate and extent of absorption estimated from the blood concentration. Depending on the agencies, the statistical methods, and the acceptance ranges for generic NTID are varied as summaries in Table 1.
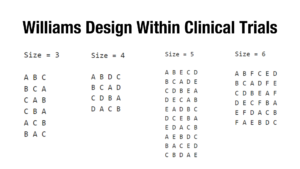
While EMA and other agencies consider narrowing the regular acceptance range from 80.00-125.00% to 90.00-111.11% for the 90% confidence interval of the geometric mean ratios of the relevant PK parameters, the FDA has defined more complicated criteria. The generic NTID must demonstrate the bioequivalence in a 4 -way, fully replicated design, regardless of its variability, and in both the regular and the reference-scaled average bioequivalence analysis. The difference in the within-subjects standard deviation between the test and reference product is also a criterion for bioequivalence assessment by FDA. The required conditions of studies also vary across countries and areas.
Interestingly enough, the complexity of bioequivalence for NTID is not in which studies to perform but if your generic product is considered as an NTID by the application-targeted agency, which might not always be straightforward as discussed earlier.
It’s worth mentioning that these are the defined criteria at the time of this blog and represent the current thinking of the agencies on this topic for general cases. Alternative approaches of sponsors with sufficient justifications and/or modified approaches by agencies to harmonize with the specific situations or the changes of thinking on the topic are expected.
What does the future hold for Narrow Therapeutic Index Drugs?
Despite the complication from drug development to therapeutic use, none can deny the essentials of narrow therapeutic index drugs. Some NTIDs are the first-line or the only available treatment option for its indication. Thus, thorough evaluations of the pipeline NTIDs safety and efficacy profiles, continuous improving the monitoring tools for approved NTIDs, and ensuring an acceptable quality of generic NTIDs as alternative treatment options are critical for all partners who are involved in “this marathon”.
With the dynamic changes from the product formulation/manufactured, product specifications testing, clinical trials conductions, treatment practices as well as the introduction of advanced models/simulations (e.g., PBPK, PK/PD model), it is expected tighter requirements for NTIDs will be required, but it will not stop the growth of these compound but promise more safe and effective treatment options for public health.
Summary of the Bioequivalence criteria per agencies
| Agency | Study design | Study condition | PK Parameter | Acceptable criteria |
| FDA3 | 4-way fully replicated crossover | Fasting and Fed | AUC and Cmax |
Must satisfy the criteria applied for all: – GMR witihin 80.00% – 125.00%, inclusively AND – Reference-replicate average bioequivalence: 95% upper confidence bound ≤ 0 AND – Regular average bioequivalence: 90% confidence interval (CI) within the 80.00% – 125.00%, inclusively AND – Within subject variability for test and treatment ratio: σWT/σWR ≤ 2.5[*] |
|
EMA4 and TGA5[†] |
Parallel, crossover | Per SmPC | AUC | Tightened range 90.00-111.11% for |
| Cmax |
– Regular range within 80.00% – 125.00% for 90% CI OR – Tightened range within 90.00-111.11% for 90% CI, if importance for safety, efficacy, or drug level monitoring. |
|||
| TPD 6[‡] | Parallel, crossover | Fast and Fed | AUC | Tightened range 90.00-111.11% for 90% CI |
| Cmax | Regular range within 80.00% – 125.00% for 90% CI | |||
| ANVISA | Parallel, crossover | Per SmPC | AUC and Cmax | Regular range within 80.00% – 125.00% for 90% CI[§] |
| NMPA | Parallel, crossover | Fast and Fed | AUC and Cmax | Regular range within 80.00% – 125.00% for 90% CI |
Developing and bringing narrow therapeutic index drugs to market is a complex and challenging process that requires careful consideration of risks and benefits. These drugs have a narrow margin between their therapeutic and toxic doses, and even small variations in dosing can have serious consequences. Therefore, additional testing and monitoring are required to ensure their safety and efficacy. This is why drug development sponsors need a reliable and experienced full-service CRO, such as BioPharma Services, that can provide a comprehensive drug development plan that takes into account the specific challenges of developing an NTID. Such a CRO can assist in risk management, study design, bioavailability, and bioequivalence testing, as well as developing a robust safety monitoring plan. With the right expertise and support, sponsors can navigate the drug development pathway for NTIDs successfully and bring safe and effective treatments to patients in need.
Why Choose BioPharma Services for drug development of narrow therapeutic index drugs?
As a full-service CRO, BioPharma Services can offer comprehensive drug development services for NTIDs to ensure their safety and efficacy. We provide services to support risk management, pharmacokinetic/pharmacodynamic (PK/PD) studies, bioavailability/bioequivalence (BA/BE) studies, and Phase 1 Clinical trials with normal healthy volunteers. By working with BioPharma Services, drug development sponsors can ensure the safety and efficacy of their NTID drugs, meet regulatory requirements, and ultimately bring their drugs to market.
[*] FDA revised this criterion to “< 2.5” in the draft Statistical Approaches to Establishing Bioequivalence Guidance in 2022. This guidance is under the “public comment” stage at the time of this blog.
[†] TGA adopted the EMA bioequivalence approach since 2011.
[‡] TPD use the term “Critical dose drugs” instead of NTIDs
[§] There is no specific criteria defined for NTIDs, thus, the regular BE criteria are applied.
Written by: Sunny Le.
BioPharma Services, Inc., a Think Research Corporation and clinical trial services company, is a full-service Contract Clinical Research Organization (CRO) based in Toronto, Canada, specializing in Phase 1 clinical trials 1/2a and Bioequivalence clinical trials for international pharmaceutical companies worldwide. BioPharma has clinical facilities both in the USA and Canada with access to healthy volunteers and special populations.