First in Human Studies for Topically Applied Drugs

What are Topical Drugs?
There is a long history of the use of topical drugs dating back to the 13th -14th centuries, where it was known that the extract from mandrake can be used together with lime to diffuse through the skin for treating stomach ulcers, constipation and reduce pain. Nowadays, there are a wide variety of prescribed topicals applied to skin, eyes, nose, mouth, gums, ears and vaginal area for the treatment of local diseases (e.g., acne [salicyclic acid, benzoyl peroxide], tinea infections [terbinafine or butenafine], psoriasis [anthralin, retinoids], and atopic dermatitis [crisaborole, tacrolimus] etc.) or for systemic conditions (e.g. hormone deficiency [testosterone], pain [fentanyl patch], Alzheimer [rivastigamine patch], etc.).
What formulations do topical drugs include?
The topical drugs come in various formats, including lotions, creams, gels, ointments, transdermal patches, sprays and powders.
Topical Drug Advantages
Topical drugs can offer certain advantages depending on if the site of action is local or the aim is to achieve systemic availability. Topical drugs, with low systemic bioavailability, can be directly applied to the affected area and allow for high local concentrations of the drug without systemic related adverse events. Topical drugs with good systemic availability have the advantage of avoiding first pass metabolism of the drug and deliver the drug through the skin at a controlled rate to the systemic circulation.
This delivery method can avoid the peak and trough concentrations seen with oral formulations and may avoid systemic adverse events seen with the peak concentration, while ensuring the drug stays within the therapeutic range.
As topical drugs offer easy administration, fewer risks of gastrointestinal difficulties and better compliance. There are numerous new drug approvals on topical drug every year. The breakdown of topical drugs approvals by FDA from 2000 through 2014 included: new dosages (64), new combinations (18), new formulations (15), and new molecular entities (NME) (14).
-
First in Human (FIH) Trial Design on Topical Drugs
FIH trials serve as the link to advance promising drug candidates (NMEs) from animal studies to human testing and into Phase II and III studies. The primary purpose for a FIH trial is to determine the safe and tolerable dosing range of the active ingredient. Typical FIH studies (oral, injection) also assess the exposure and pharmacokinetic profile of the active ingredient and active metabolite of the study drug.
The regulatory pathway for new topical drugs varies depending on whether the topical drug is with an NME or is repurposed from an already established formulation or is a generic drug. The data required by regulatory agencies for topical drugs with NMEs will be dependent on whether the topical drug is aiming for local conditions or for systemic exposure.
Typically, FIH trials of topical drugs with NMEs aiming for systemic exposure would be evaluated through oral or injection routes, and the topical formulations may be assessed later.
Here we will mainly discuss topical drugs with NMEs for local conditions.
For topical drugs where the aim is to avoid systemic exposure, a critical safety consideration for FIH trial on topical drugs is to identify to what extent that the topical drug result in systemic exposure to the active ingredient. Thus, there are some specific elements that should be taken into considerations for FIH study design on topical drugs.
A. Study Population
Traditional first in human trials for systemic drugs are often conducted on healthy volunteers. However, FIH studies for topical drugs can include healthy subjects or patients or even both, which depends on the therapeutic indications and risk-to-benefit profiles. The reason that patients may be suitable to enrol in a FIH study for a topical drug is because there will be fewer concerns of systemic adverse events due to the expected low systemic exposure. Furthermore, studies in subjects with healthy skin may not be relevant for local conditions and there may be differences in systemic absorption of drug through intact healthy skin versus skin affected by a disease condition.
Possible interactions between the topical drugs and subject age, gender, concomitant medications, lifestyle and genotypes have impacts on the inclusion of subjects. For skin applied drugs, skin elasticity, vascularity, moisture content should be representative for the population expected to be treated. The relatively larger ratio of skin surface to body volume and thinner stratum corneum in younger subjects may increase systemic exposure compared with elderly population.
B. Sample Size
Most FIH trials are blinded, placebo-controlled, dose escalation studies. Similar design is applied for FIH studies on topical drug as would be used for oral studies. There is no general agreement on the cohort size. Usually, it is reasonable to have 8 to 10 subjects per cohort randomized in a 3:1 or 4:1 ratio for active therapy vs placebo.
C. Starting Dose, Dose Escalation Scheme and Stopping Criteria
In regard to the administration of topical drugs, doses (including mass or volume of drug product), surface area to be treated, application method and site preparation should be specified and justified in the FIH study protocol.
It is critical to translate the dose from animal data to the doses to be used in the FIH study. For systemic drugs, the traditional way to do the dose extrapolation is to follow the FDA guidance for estimating a maximum safe starting dose by converting NOAEL obtained from the most sensitive animal toxicology test to HED based on body surface area (BSA)-related scaling or similar mathematical paradigms.
For topical drugs, however, bioavailability and metabolism of the active ingredient may differ significantly between human and animals. Hence, there are more considerations than NOAEL that need to be taken into account for the safe starting dose selection for topical drugs. Usually the following consideration should be taken into account during preclinical stage of the development plan of topical drugs:
-
- Preclinical safety assessment should be performed in a rodent and a non-rodent species to measure systemic and topical exposures as well as toxicity by the intended route of administration;
- Safety pharmacology studies on CNS, respiratory system and in vitro hERG, etc. should be conducted;
- Genotoxicity needs to be addressed; (4) in particular for topical drugs, local safety such as irritation, sensitization and photo safety are generally required to be conducted with the to-be-marketed formulation and strength.
Dose escalation decision in FIH trials is based on balancing safety risks against the risks of failing to define the correct dose by assessing safety and PK profile at a lower dose. This is needed even if systemic exposure is expected to be limited, and particularly if the NME may demonstrate toxicity even at low exposure.
For topical delivery system, most of the time it is not feasible to assess the target site pharmacokinetics (PK). Thus, how to determine the maximum tolerated dose (MTD) of topical drug is to designate what toxicities are important per nonclinical studies. They can be lab test (e.g., AST, ALT, GGT, creatinine etc) or clinically significant symptoms (vomit, dizzy, diarrhea etc.).
The topical drugs are designed to be effective at a localized site, ideally offers avoidance of severe systemic adverse events (AEs). Meanwhile, at the site of action, the nature of the drug and excipients in conjunction with the condition of the skin, may irritate the skin or lead to a sensitization reaction. Therefore, the stopping criteria in a FIH trial for topical drug should take both systemic and local AEs into consideration. On one side, clear stopping rules must be established for stopping the drug administration by defining the severity level and the number of systemic or local AE occurrences; on the other hand, the stopping rules should avoid stopping dosing or dose escalation when it is not warranted.
Example; non–steroidal anti–inflammatory drugs (NSAIDs) when applied topically, reduce the pain mainly through local anti–inflammatory effects. If there are occurrences of systemic AEs such as seizure, drowsiness or hypertension etc., even one severe AE deemed related to the study drug may also result in a temporary halt of dosing. It should also be considered if unexpected PK levels or systemic AEs are consistent with further drug development.
Systemic PK levels or even mild systemic AEs may not warrant further drug development for some topical drugs. One thing to note that, in order to evaluate the relatedness of AE to the study drug and AE to the excipients, placebo control is necessary to be built in the study design
Even for topical drugs treating local conditions, the area to apply the drug needs to be carefully considered. The drug should only be applied to the affected area in the patients or the expected affected area in the healthy participants. Considerations should be made about how large the affected area of skin treated may be and how this impacts overall exposure.
The concentration and thickness of drug may be kept constant, but dose escalation to assess systemic PK and safety may be achieved by applying the drug to a larger area. In addition, the efficacy of the drug may be assessed with higher concentrations or thickness of the drug application. Again, the impact of treating a larger area of skin with higher amounts per area need to be considered. Extra precaution should be taken if the area to be treated are armpits.
The area of skin where the topical drugs are applied can impact local and systemic effects. Elbows and knees have different skin thickness than the forearm or stomach. Age and skin type can also have a big impact on drug absorption.
Example; the topical application should be done sparingly as armpits absorb more medication than other parts of the body due to the skin in this area is thin and rub together. In addition, it is essential to ensure a consistent amount of drug is applied each time by cleaning the skin before applying a new dose of topical drugs and applying the dose on a consistent surface to ensure even medication distribution. The area of skin to be treated may be marked.
D. Safety Endpoints
To confirm safety and tolerability of the investigational product is the primary objective in a FIH study on topical drugs.
Even for NME intended to treat local conditions, a systemic safety evaluation should include assessments of AEs, lab data, physical examination, vital signs and ECG when appropriate. For investigational topical drug with NME indicated for local conditions, when a particular AE, e.g., the abnormal hepatic transaminases, is observed from both preclinical and clinical studies, a detailed history of recent intake of alcohol and other medications more than a simple AE description will be more helpful in determining causality.
Topically applied analgesics are always associated with site reactions such as dryness, erythema, burning, and discoloration. Hence, in addition to conventional systemic safety assessment, skin irritation, sensitisation, adhesion, are also important assessments to be considered into FIH study design on topical drugs .
E. Pharmacokinetics (PK) Endpoints
Generally, a topically administered drug intended for local effect has very little systemic absorption due to the barrier function of the thick outer layers of the stratum corneum.
Example; topical nonsteroidal anti-inflammatory drug, derivatives of acetylsalicylic acid, patches and creams containing local anesthetic act more directly on the affected tissue without interfering systemic circulation. However, it cannot be assumed that all topical drugs have little systemic absorption. Other mroe classical examples are topically applied corticosteroids, which may lead to blood concentrations high enough to cause Cushing’s syndrome, diabetes mellitus, hyperglycaemia and cortisol suppression.
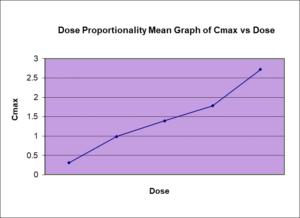
Thus, the systemic exposures to the active ingredients or clinically relevant metabolites should be evaluated by using standard PK parameters, such as Cmax, Tmax, AUC and T1/2 and the link between the systemic exposure and the systemic AEs observed at a certain dose level can help to define the maximum acceptable systemic exposure and identify stopping criteria from PK’s perspective.
F. Clinical and Pharmacodynamic Endpoints
The clinical endpoints in topical drugs FIH studies are based on the proposed indications.
Example; if the investigational topical drugs are indicated for complicated vascular anomalies and other susceptible lesions, reduction in pain or local irritation and decrease in cyst formation will be the main clinical endpoints. If the study drug is for topical anesthesia, the efficacy of topical anesthetics on the application site can be assessed by mechanical touch and pain sensory evaluations using the Von Frey Filament and PinPrick methods, respectively.
It is worthy to note that the implementation of a biomarker in topical drug FIH study can be valuable to the drug development. A well-defined biomarker can enable a solid dose rationale and make an appropriate evaluation of proof of concept. The biomarkers can be from various matrices such as serum, plasma, ocular fluids, tissue biopsies etc. Take a skin repair drug as an example, Ki67 is the well-established marker to probe cellular proliferation during wound repair, Ki67 in skin biopsy samples can be taken as the biomarker to assess the cell proliferation extent.
G. Other Considerations
A good study design of a FIH trial is key to the early phase development of a topical drug and help provide important of the Phase II and III clinical development plan. Topical drugs studies with low systemic exposure can include other design elements that are not possible with oral or injection studies. In addition to having placebo only treated subjects, active subjects could be treated with active and placebo on, for example, opposite arms. The subject can then be used as their own control (if applicable) to normalize the safety and efficacy data in different ways during the data analysis stage.
This is especially helpful if there is a high natural variability relative to a smaller treatment effect. Normally, with a good sample size, the differences between mean placebo treated against mean active treated can be identified. However, if the sample size is small and the variability between subjects is high, having subjects serve as their own control will be very useful, as we can tell the difference between untreated/vehicle treated area and treated area in the same subject at the same time.
Normalizing for both can take some of the background variability out. The placebo only treated subjects can also help to tease out the natural differences over time and between different untreated areas. The advantages of such study design are to give a better understanding of the treatment effect size, dose levels and natural variability (within and between subjects), provide flexible approaches to analyze the data to determine the drug effect as well as help for the development of late phase protocols.
Why Choose BioPharma Services?
Topical drugs have been used for centuries and come in various formats including lotions, creams, gels, ointments, transdermal patches, sprays, and powders. These drugs offer advantages such as easy administration, lower risks of gastrointestinal difficulties, and better compliance. First in human (FIH) trials serve as the link between animal studies and human testing to determine the safe and tolerable dosing range of the active ingredient.
When enrolling patients in a FIH study for topical drugs, various factors need to be considered, such as age, skin type, and the potential for both systemic and local adverse events etc. A comprehensive systemic safety evaluation should be conducted, even for NMEs intended to treat local conditions. The use of a biomarker in the FIH study can also be valuable for drug development. Overall, topical drugs provide a valuable option for the treatment of local and systemic conditions, and FIH trials are essential in advancing the development of these drugs.
Written By: Vivian Zha
Find out why BioPharma might be the right partner for you! Learn more about BioPharma Services and the wide array of bioanalytical services we provide.
BioPharma Services, Inc., a Think Research Corporation and clinical trial services company, is a full-service Contract Clinical Research Organization (CRO) based in Toronto, Canada, specializing in Phase 1 clinical trials 1/2a and Bioequivalence clinical trials for international pharmaceutical companies worldwide. BioPharma has clinical facilities both in the USA and Canada with access to healthy volunteers and special populations.