Navigating ANVISA’s Requirements: A Guide to Performing and Analyzing Bioequivalence Studies for the Brazilian Health Authority

In the realm of pharmaceutical research and development, ensuring the safety and efficacy of drugs is of paramount importance. Bioequivalence (BE) studies play a crucial role in this process for generic drug development, and regulatory bodies like the Brazilian Health Regulatory Agency, known as ANVISA (Agência Nacional de Vigilância Sanitária), set forth stringent requirements to ensure the quality and interchangeability of generic and branded drugs.
The Brazilian market for bioequivalence generic products is significant and continues to grow. Brazil has a large population and a robust pharmaceutical market, making it an attractive market for generic drug manufacturers. The Brazilian government has implemented policies to promote the use of generic drugs in the country, aiming to increase accessibility and reduce healthcare costs. These policies include measures such as the requirement for doctors to prescribe by the International Nonproprietary Name (INN) instead of brand names and the establishment of a bioequivalence study requirement for generic drug approval.
In this blog, we’ll take a closer look at ANVISA and what it requires for conducting bioequivalence studies.
What is ANVISA?
ANVISA is the regulatory agency responsible for supervising, controlling, and promoting public health within Brazil. It operates under the Ministry of Health and plays a vital role in ensuring the safety, efficacy, and quality of health products, including pharmaceuticals, medical devices, and cosmetics. ANVISA’s primary objective is to safeguard public health by regulating and overseeing the entire lifecycle of health products, from manufacturing and distribution to post-marketing surveillance.
Bioequivalence Studies and their Importance
Two products are bioequivalent when they are equal in the rate and extent of absorption to which the active pharmaceutical ingredient (API) becomes available at the site(s) of drug action when administered at the same molar dose under similar conditions. Bioequivalence studies are conducted to establish the pharmaceutical equivalence between two drugs, most often ensuring that the generic drug performs in the same manner as the approved reference drug. These clinical studies are crucial to confirm that generic drugs are safe, effective, and can be used as a substitute for their branded counterparts.
ANVISA Requirements for Bioequivalence Studies
ANVISA mandates that clinical sites and analytical labs involved in bioequivalence studies must undergo certification by the agency per their RDC 620-2022 guidelines for certification. The certification process entails evaluating various aspects such as infrastructure, equipment validation, verification of analytical methods, implementation of quality control measures, personnel qualifications, and adherence to good clinical practices (GCP).
Certification serves as a guarantee that the site meets ANVISA’s rigorous standards for conducting research, ensuring the reliability and validity of study results. Furthermore, ANVISA’s certification ensures that the laboratory operates under robust quality assurance systems, ensuring the accurate and precise analysis of study samples. In the case of BioPharam Services Inc. (BPSI), both our clinic and lab facilities located in Toronto, Canada, as well as our clinic site in St. Louis, USA, have successfully obtained certification from ANVISA.
Brazil is an official member of the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) and follows ICH guidelines. ANVISA has established a comprehensive set of requirements for conducting bioequivalence studies in Brazil in line with ICH guidelines. These bioequivalence requirements are designed to ensure the reliability and validity of the study results, ultimately guaranteeing the safety and efficacy of generic drugs. Most of the major criteria for conducting the bioequivalence studies for generic products are similar among different regulatory agencies; however, they have some differences.
Table 1- Similarities and Differences in Regulatory Requirements for Bioequivalence Study of Generic Products (ANVISA, FDA, EMA, TPD and WHO)
| Criteria | Agencies | ||||
|
ANVISA (Brazil) |
FDA (USA) |
EMA (Europe) |
TPD (Canada) |
WHO (World Health Organization) |
|
| General Criteria | |||||
| Age | 18 -50 years old, inclusive | 18 years and older | 18 years and older | 18-55 years old, inclusive | Not specified as long as subjects are defined as healthy |
| Sex | Both Sex Numbers of males and females be distributed equally among the sequence | Both Sex unless there is a significant risk on a specific sex | Both Sex unless there is a significant risk on a specific sex | Both Sex unless there is a significant risk on a specific sex | Both Sex unless there is a significant risk on a specific sex |
| BMI | ± 15% of the normal BMI | Not specified | 18-30 kg/m2, inclusive | ||
| Smoking | Non-smoker is preferable | Non-smoker is preferable | Non-smoker is preferable | Non-smoker is preferable | Non-smoker is preferable |
| Exclusion Criteria | Subjects must not participate in a clinical research study for 6 months prior to study commencement | It is acceptable that subjects do not participate in a clinical research study for at least 30 days prior to study commencement | It is acceptable that subjects do not participate in a clinical research study for at least 30 days prior to study commencement | It is acceptable that subjects do not participate in a clinical research study for at least 30 days prior to study commencement | It is acceptable that subjects do not participate in a clinical research study for at least 30 days prior to study commencement |
| Present of Physician | During the whole confinement period at the clinic site |
It is acceptable: 30 minutes prior to dosing until a minimum of 4 hours after the last subject is dosed. The Physician can remain on-call throughout the duration of the study. |
It is acceptable: 30 minutes prior to dosing until a minimum of 4 hours after the last subject is dosed. The Physician can remain on-call throughout the duration of the study. |
It is acceptable: 30 minutes prior to dosing until a minimum of 4 hours after the last subject is dosed. The Physician can remain on-call throughout the duration of the study. |
It is acceptable: 30 minutes prior to dosing until a minimum of 4 hours after the last subject is dosed. The Physician can remain on-call throughout the duration of the study. |
| Blinding | Open-label | Open-label | Open-label | Blinded | Open-label |
| Strength | Highest or most sensitive strength | Highest or most sensitive strength | Highest or most sensitive strength | Highest or most sensitive strength | Highest or most sensitive strength |
| Moieties to Measure |
Parent (Measuring metabolite to be assessed by ANVISA case by case per approval by ANVISA) |
Parent (active ingredient or active moiety) + active metabolite as supportive evidence | Parent (active ingredient or active moiety) | Parent (active ingredient or active moiety) | Parent and/or metabolite |
| Fasting Period for Fasting Studies | Not specified. Generally, 8-10 hours | FA: overnight fast of at least 10 hours. | FA: overnight fast of at least 8 hours. | FA: overnight fast of at least 8 hours. | Not specified. Generally, 8-10 hours |
| Breakfast for Fed Study | High-fat meal 30 minutes prior to dosing | High-fat meal 30 minutes prior to dosing | High-fat meal 30 minutes prior to dosing | High-fat meal 30 minutes prior to dosing | High-fat meal 30 minutes prior to dosing |
| Volume of Water with Dosing | 200 mL | 240 mL | At least 150 mL | 150-250 mL | 180-240 mL |
| Water Restriction | allowed water as desired except for dosing and 1 hour before to 1 hour after drug administration | allowed water as desired except for dosing and 1 hour before to 1 hour after drug administration | allowed water as desired except for dosing and 1 hour before to 1 hour after drug administration | allowed water as desired except for dosing and 1 hour before to 1 hour after drug administration | allowed water as desired except for dosing and 1 hour before to 1 hour after drug administration |
| Some of the Pharmacokinetic and Statistical Criteria | |||||
| Duration of PK Sampling | Equal to or greater than 3-5 times the elimination half-life of the analyte | At least 3 times the elimination half-life of the analyte | Long enough that AUC(0-t) covers at least 80% of AUC(0-∞). which is around 3 half-lives | At least 3 times the elimination half-life of the analyte | |
| Washout | At least 7 elimination half-lives | At least 5 elimination half-lives | At least 5 elimination half-lives |
Not less than 10 times the mean terminal half‐life |
At least 5 elimination half-lives |
|
Truncated Approach (AUC72) |
Accepted for a product with a long half-life of more than 24 hours | Accepted for a product with a long half-life of more than 24 hours and not exhibiting flip-flop kinetics | Accepted for a product with a long half-life of more than 24 hours | Accepted for a product with a long half-life of more than 24 hours | Accepted for a product with a long half-life of more than 24 hours |
| Pre-dose 5% > Cmax |
Data from the subject will be and excluded from the PK/stats analysis. |
Data from the subject will be excluded from the PK/stats analysis. |
Data from the subject will be excluded from the PK/stats analysis |
Data from the subject will be excluded from the PK/stats analysis |
Data from the subject will be excluded from the PK/stats analysis |
| Timepoints used for PK analysis |
The calculations with nominal times and actual times will be presented in the report. PK parameters calculated with nominal times will be used for BE assessment. |
Actual times to be used to calculate PK parameters. | Actual times to be used to calculate PK parameters. | Actual times to be used to calculate PK parameters. | Actual times to be used to calculate PK parameters. |
Table 1 summarizes some of the similarities and differences among ANVISA, Food and Drug Administration (FDA), European Medicine Agencies (EMA), Health Canada, Therapeutic Products Directorate (TPD) and World Health Organizations (WHO) for generic bioequivalence studies which are essential. The exception may be applied to specific drug formulations with different characteristics such as variability, PK, and safety properties. Here are some key aspects of ANVISA’s requirements for bioequivalence studies, which should be outlined in the study protocol per ICH and specific listed ANVISA guidelines:
-
- RE_1170_2006_Guide for Relative Bioavailability Bioequivalence of Medication Tests,
- RE_894_2003_Guide for preparing a BABE Study Protocol
- RDC 27-2012 Bioanalytical Guidance
- RE_898_2003_Guide for Planning and Carrying Out the Statistical Stage of BABE Studies and
- RE_895_2003_Guide for Preparing a Technical Study Report.
Study Design and Sample Size:
Conventional bioequivalence studies for ANVISA follow an open-label, randomized, crossover design, which is detailed in the study protocol. Participants receive the test and reference drugs on separate occasions (periods), in a single or multiple-dose schedule. Parallel design can be used, when necessary, similar to other regulatory agencies. The washout period between the dosing of the test and reference product should be at least seven times the elimination half-lives of the study drugs to eliminate any potential carryover effects. You can find out about the minimum washout required by some of the agencies in Table 1.
The bioequivalence study should also include an appropriate sample size, which is determined based on statistical power calculations. The chosen sample size should ensure the study has enough 80% statistical power to detect relevant differences between the reference and test products, similar for all regulatory agencies.
Dosing and Administration:
Similar to the other regulatory agencies, the protocol for ANVISA should outline the dosing regimen for the reference and test products, including the dose strength, frequency, and duration of administration. It should also specify any restrictions on concomitant medications or dietary considerations during the study period. However, the dosing water recommended by ANVISA is 200 mL, which is slightly different from the conventional amount of 240 mL
Reference and Test Product Selection:
ANVISA requires the selection of the highest strength reference product and test product, like other regulatory agencies. The reference product is typically an approved and marketed innovator drug in Brazil. The test product, a generic version, should contain the same active ingredient(s), strength, dosage form, and route of administration as the reference product.
Unlike other regulatory agencies, ANVISA requires the certificate of Pharmaceutical Equivalence of the study drugs to be presented by the sponsor, which also includes the difference between the test drug and reference drug. The study should not be started with products that have differences greater than 5%.
Study Population:
ANVISA specifies the characteristics of the study population participating in bioequivalence studies. The population should generally consist of non-smoker healthy individuals of both sex, male and female which number of males and females be distributed equally among the sequence, within a specific age range of 18 to 50 years old with body weight ± 15% of the normal body mass index (BMI)). In some cases, studies may require specific populations if the drug is intended for a particular patient group. You can check Table 1 for the requirements of other agencies.
Sampling Procedures and Analytical Methods:
ANVISA like other regulatory agencies requires detailed instructions for blood or plasma sampling procedures, including the time points for sample collection after drug administration indicated in the study protocol or study-specific lab documents such as manual, directive or report. The protocol should specify the analytical methods to be used for determining the drug concentrations and pharmacokinetic parameters.
ANVISA specifies that analytical methods used in bioequivalence studies should be validated according to the ICH guidelines ICH M10 and ANVISA guideline RDC 27-2012 Bioanalytical Guidance. These methods should demonstrate appropriate sensitivity, specificity, accuracy, and precision to ensure reliable and reproducible results.
Statistical Analysis:
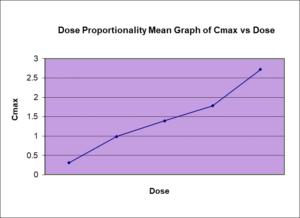
Bioequivalence studies should evaluate relevant pharmacokinetic parameters to establish bioequivalence. The protocol should outline the appropriate statistical analyses to compare the pharmacokinetic parameters of the reference and test products, including the area under the concentration-time curve (AUC), maximum concentration (Cmax) and time to reach the maximum concentration (Tmax). Similar to other regulatory agencies such as FDA, EMA and WHO, ANVISA considers two products bioequivalents if the 90% confidence interval for the ratio of the geometric means of the test-to-reference product falls within the acceptance range of 80-125% for both the AUC and Cmax.
Statistical methods such as analysis of variance (ANOVA) or linear mixed-effects models are required to be used to assess bioequivalence. Unlike other regulatory agencies, the 90% confidence interval for median Tmax using a non-parametric Test is also required by ANVISA.
Safety and Adverse Events Monitoring:
The protocol should include provisions for monitoring and reporting adverse events and any safety concerns during the study. This ensures participant safety and compliance with ethical standards.
According to ANVISA’s regulations, it is mandatory for a physician, who has received training in the study protocol, to provide continuous assistance to the study participant during their entire confinement period at the clinic site. Additionally, ANVISA allows a delegated physician assistant, who has also been trained in the study protocol, to offer evening/overnight coverage for the study throughout the entire period of
Data Management and Quality Assurance:
ANVISA expects clear guidelines for data management, including collecting, storing, and analyzing study data similar to other regulatory agencies. The protocol should also address quality assurance measures to ensure data accuracy and integrity.
Reporting:
ANVISA has specific requirements for the clinical study report (CSR) submitted as part of the bioequivalence study documentation (RE_895_2003_Guide for Preparing a Technical Study Report). ANVISA accepts the ICH E3 requirements for the full and abbreviated CSR. The CSR comprehensively summarizes the bioequivalence study design, methods, results, and conclusions. The report should also address any deviations from the study protocol and provide justifications for these deviations, like other regulatory agencies. Here are some key ANVISA requirements for CSR:
- Study Information and Background:
The CSR should provide a clear overview of the study, including the study title, objectives, rationale, and background information about the drugs being compared. It should also include a summary of previous studies or relevant literature that supports the need for a bioequivalence study.
- Study Design and Methods:
The CSR should detail the study design and the methodology used for study participant selection, randomization, blinding, and allocation concealment. It should also describe the dosing regimen, administration procedures, and any specific instructions given to participants during the study.
- Participant Characteristics:
The CSR should provide information about the study population, including the number of participants enrolled, demographic characteristics, inclusion/exclusion criteria, and any baseline characteristics relevant to the study objectives.
- Pharmacokinetic Assessments:
Detailed information about the pharmacokinetic assessments conducted during the study should be included in the CSR. This includes the sampling schedule, methods used for blood or plasma sample collection, analytical methods employed for drug concentration analysis, and any adjustments or exclusions made for non-compliant samples.
- Statistical Analysis:
ANVISA requires a thorough statistical analysis section in the CSR. It should outline the statistical methods used to analyze the pharmacokinetic data, including the calculations of means, standard deviations, and confidence intervals. The analysis should also include any relevant statistical tests used to compare the reference and test products.
- Results:
The CSR should present the study results in a clear and concise manner. This includes the summary of the pharmacokinetic parameters for both the reference and test products. The results section should also include any relevant statistical analyzes, including p-values and confidence intervals.
- Discussion and Conclusions:
ANVISA expects a comprehensive discussion of the study findings and their implications in CSR. This section should compare the results of the reference and test products, assess the bioequivalence based on the predetermined acceptance criteria, and discuss any potential factors that may have influenced the study outcomes. The CSR should conclude whether the products are considered bioequivalent or not based on the results.
- Safety and Adverse Events:
The CSR should include a detailed summary of safety data and adverse events observed during the study. This includes any reported adverse events, their severity, and their relationship to the study drugs. Any safety concerns or notable findings should be thoroughly discussed in this section.
- Compliance with Good Clinical Practice (GCP):
ANVISA emphasizes the importance of adherence to good clinical practice (GCP) guidelines throughout the study and in the CSR. The CSR should demonstrate that the study was conducted in compliance with ethical principles, participant protection, data integrity, and regulatory requirements.
Why Choose BioPharma Services?
By adhering to these ANVISA requirements, pharmaceutical companies can ensure that their bioequivalence studies meet the necessary standards for regulatory approval, demonstrating the safety and efficacy of generic drugs in Brazil. It is essential for researchers and sponsors to consult the specific ANVISA guidance documents for detailed and up to date. Compliance with these requirements ensures that the report meets ANVISA’s standards and supports the regulatory evaluation of the bioequivalence of the tested products. BioPharma Services has successfully conducted several studies for the ANVISA submission. If you’d like to understand our capabilities and experience, contact one of our expert scientific team members for your next drug development project. BioPharma Services can help guide your next clinical drug development project from concept to clinic.
Written By: Negar Gharavi, Senior Director Medical Writing & Regulatory Affairs
BioPharma Services, Inc., a Think Research Corporation and clinical trial services company, is a full-service Contract Clinical Research Organization (CRO) based in Toronto, Canada, specializing in Phase 1 clinical trials 1/2a and Bioequivalence clinical trials for international pharmaceutical companies worldwide. BioPharma has clinical facilities both in the USA and Canada with access to healthy volunteers and special populations.