Rare Diseases: Genetic Epilepsies – A New Frontier For Drug Development

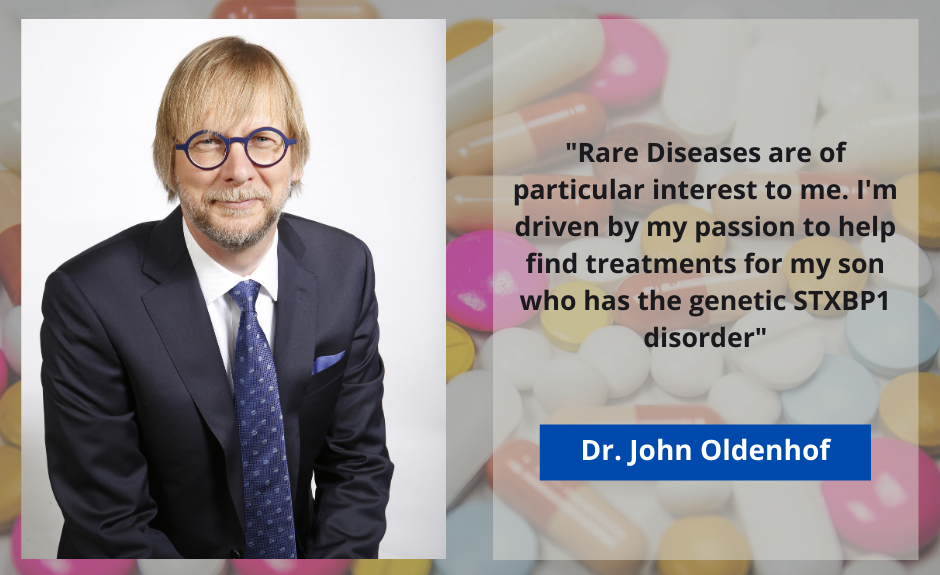
By Dr. John Oldenhof, Chief Scientific Officer, BioPharma Services Inc.
Note, a short glossary of some uncommon terms is included at the end of the article.
Rare Diseases, and in particular Genetic Epilepsies, are of particular interest to me. It is where my different passions and experience overlap. My interest in genetics and neuromolecular pharmacology was fostered (1) during my PhD studies, (2) my 20 years in drug development working on First-in-Human and Clinical Pharmacology studies, and most importantly (3) my passion to help find treatments for my son, who has the genetic STXBP1 disorder. STXBP1 is a 1 in 30,000 condition that impairs the release of neurotransmitters from the synapse resulting in epilepsy and profound cognitive impairment. Genetic epilepsies are good examples of how drug development is improving for rare diseases.
Genetic epilepsies are a new area of drug development that has been receiving a lot of attention in the last few years. In the last century, the etiology of a large proportion of epilepsies was not known; they could not be attributed to physical abnormalities in the brain or as a result of brain trauma, and many were multifocal in origin. Many of these epilepsies have an onset in infancy, are severe, intractable, and also lead to significant development issues. These epilepsies are treated with traditional epilepsy medications, many targeting the GABA system and do not consider the underlying cause, but mediate excitability of the central nervous system (CNS). What might be considered late, relative to other rare disease conditions, the advent of genetics has in the last decade or so identified a multitude of single gene causes of epilepsies.
What were originally classified as syndromes (Dravet, Ohtahara, Lenox Gastaut) and were classified by their clinical presentation, are now being classified and categorized by the gene and protein that is the cause of the disease. Many of the epilepsies are caused by variants in ion channels involved in propagating action potentials and others are caused by proteins in the synapse that are critical to the normal release of neurotransmitters. Identifying these proteins has increased the druggable targets. We can now target specific proteins that are impacted or identify the pathways these proteins participate in, in order to manipulate them. It may be, that some of the medications that are developed for these specific genetic epilepsies may have use for seizure disorders in general and provide new types of drugs that may be more effective than the current repertoire of about 30+ approved drugs.
Estimates are that there are about 7,000-10,000 different rare diseases, with most rare diseases having a genetic basis. Although the number of rare disease treatments are increasing – the FDA approved 21 novel drugs in 2015 and 48 in 2019 for rare or orphan indications – there is a long way to go before the thousands of rare diseases have an approved treatment. With personalized medicine, the potential and advantage of finding specific treatments to “cure” some of these rare diseases is hampered by the small number of patients that these specific drugs would benefit.
Central to the push for new treatments for rare diseases are Patient Advocacy groups. These are generally started and supported by parents. They are the link between the patients, the doctors and the drug developers. Using social platforms such as Facebook to connect across the globe, the collective knowledge that parents have often exceeds the clinical knowledge of the individual specialists that treat our children. They help to organize the scientific meetings that brings clinicians and scientists together, do fundraising to help fund academic research and they provide the critical mass of patients that piques the interest of the pharmaceutical industry. Patient advocacy groups help establish patient registries which are both important to learn as much about the disease as possible, and to provide a database of patients ready to participate in clinical studies.
There are a number of different approaches to developing drugs for rare diseases. This is aided by the FDA and other regulatory agencies that make allowances for a reduced drug development burden for these orphan indications which impact a small number of patients but at the same time may produce a severe disease burden. “n” of 1 studies are also being used in the ultimate personalized medicine approach, but requires detailed natural history studies to fully understand the progression of the disease and to determine if treatment has an impact on the disease progression.
Drug repurposing is the fastest approach to getting much needed drug treatments to patients. Through the use of drug screens, Artificial Intelligence (AI) and animal models that display phenotypes of the genetic disease, already approved drugs are identified that may impact some, or all, of the symptoms of the disease. These could be through mechanisms distinct from the original indication. With strong scientific evidence, this may lead to early availability through off label use, or can be developed into an approved drug through the FDA’s 505(b)(2) application, or a similarly shortened approval process in other regulatory jurisdictions, that relies on already available preclinical and clinical data.
Small molecule, Novel Chemical Entities (NCE), drug development is now possible that targets the new pharmacologic sites identified. Early preclinical research is aided with animal models of the rare disease that express the phenotype and serve as a model to demonstrate efficacy. For genetic epilepsies, in vitro models (e.g. iPSCs – induced pluripotent stem cells from individual patients) and animal models in c.elegans, zebra fish, and mouse often show seizure activity that can be treated with traditional epilepsy medications and new candidates.
By far the most interesting exciting area of drug development is related to genetic therapies. Multiple strategies are being developed to impact the expression of genes. This can involve the down-regulation of the pathogenic gene variant or the up-regulation of the normal gene variant. Strategies to introduce mRNA to express wild type gene variants are being developed, with the major challenge of getting the mRNA across the Blood Brain Barrier (BBB) and into neurons safely. Other strategies include various methods using antisense oligonucleotides (AS) including small interfering RNA (siRNA) to prevent the expression of the mRNA leading to the defective protein.
There are also strategies where the offending portion of the pathogenic protein are not transcribed and drugs for Skeletal Muscle Atrophy (SMA) have recently been approved using this approach. Probably the most promising, but also furthest away from implementation is correcting the gene variant through the use of CRISPR and/or base editing technologies early in the patients’ development to cure the disease and lead to normal development. More development is needed before the first attempts to use this technology can be safely done in humans, especially for CNS diseases. However, once this technique is developed for one condition, it can be readily applied to the many rare diseases.
Significant obstacles exist to developing drugs for rare and especially ultra rare diseases. In addition to the extraordinary costs to produce medicines for such a small number of patients, the fact that there are only a few patients makes recruiting for these studies challenging. Some companies are adopting an approach of performing many of these studies in healthy volunteers in order to “save” the patients for those studies aimed at demonstrating efficacy. On the positive side, as these alternate ways of treating disease are established to be safe, the technological advances and established safety profile should make the drug development process more streamlined for future products using the same platform. Genetic epilepsy is benefiting from early development work in other rare diseases. Likewise, conditions such as STXBP1 are benefiting from what is being learned by some of the other more common genetic epilepsies, that already have drug candidates in clinical trials.
First-in-Human clinical studies in Early Phase or Phase I development, need special considerations especially for genetic therapies. In addition to the on-target effect of down or upregulating a specific protein, the safety risks with the delivery technology or platform (e.g. adeno virus, molecular modification, lipophilic vesicles) needs to be considered. Intravascular (IV) or intramuscular injections can result in infusion reactions and has the potential for anaphylactic shock. Our scientific and medical team carefully assesses the inherent risks and we rely on past studies to guide appropriate safety monitoring, confinement and potential medical intervention that is needed. In Canada, Health Canada has been approving these studies for a number of years and carefully reviews these protocols with safety in mind.
BioPharma Services is excited to be involved in the early development of genetic therapies for rare diseases. Personally, it is rewarding to be able to contribute to the development of drug therapies for my son’s condition as well as rare diseases in general.
See list of BioPharma Services clinical trials here
References
STXBP1 Disorder Foundation
Beyond the Ion Channel
Overview of Rare Diseases: Sen et al., 2017
FDA Rare Disease Drug Approvals
BioPharma Services Rare Disease clinical trials
Glossary
c.elegans Caenorhabditis elegans is a free-living transparent nematode that lacks respiratory or circulatory systems which lives in temperate soil environments.
Dravet syndrome An autosomal dominant genetic disorder which causes a catastrophic form of epilepsy, with prolonged seizures that are often triggered by hot temperatures or fever. In 80% of the cases it is caused by mutations in the sodium channel SCN1A gene. Previously known as severe myoclonic epilepsy of infancy (SMEI).
Etiology The cause, set of causes, or manner of causation of a disease or condition.
FDA 505(b)(2) application A 505(b)(2) application is a new drug application (NDA) described in section 505(b)(2) of the Federal Food, Drug, and Cosmetic Act. This type of application allows a sponsor to have some safety and efficacy information on the active ingredient to come from studies not conducted by or for the applicant.
GABA system The GABA receptors are a class of receptors that respond to the neurotransmitter gamma-aminobutyric acid (GABA), the chief inhibitory compound in the mature vertebrate central nervous system
iPSCs (induced pluripotent stem cells) A type of pluripotent stem cell that can be generated directly from a somatic cell.
Lennox–Gastaut syndrome (LGS) A complex, rare, and severe childhood-onset epilepsy. It is characterized by multiple and concurrent seizure types, cognitive dysfunction, and slow spike waves on electroencephalogram (EEG).
mRNA The form of RNA in which genetic information transcribed from DNA as a sequence of bases is transferred to a ribosome.
Ohtahara syndrome (OS) A progressive epileptic encephalopathy. The syndrome is outwardly characterized by tonic spasms and partial seizures within the first few months of life, and receives its more elaborate name from the pattern of burst activity on an electroencephalogram (EEG). Also known as early infantile epileptic encephalopathy (EIEE).
Synapse A junction between two nerve cells, consisting of a minute gap across which impulses pass by diffusion of a neurotransmitter.
About the Author
Dr. John Oldenhof is the Chief Scientific Officer at BioPharma Services. John joined the BioPharma team in 2018 and brings with him 18 years of senior management experience in Phase I clinical pharmacology, product development, biostatistics, data management and regulatory and scientific affairs. His published work and experience includes the development of novel methodologies, innovative study designs and direct collaboration with the US Food and Drug Administration (FDA) to advance human abuse potential studies and pharmacometrics analyses.
Dr. Oldenhof holds an Adjunct Lecturer position in the Department of Pharmacology & Toxicology at the University of Toronto
Dr. Oldenhof is a parent member of the STXBP1 disorder Scientific Advisory Board
Over his tenure in Clinical Pharmacology, Dr. Oldenhof has provided scientific and regulatory guidance to biotech and pharmaceutical sponsors on over 250 clinical pharmacology studies including FIM, SAD/MAD, DDI, TQT and Human Abuse Potential (HAP) studies to support pre-IND, NDA, ANDA and product launches.
About BioPharma Services Inc.
BioPharma Services Inc. is a full-service Contract Research Organization (CRO) specializing in the conduct of Phase I/IIa and Bioequivalence clinical trials for international pharmaceutical companies worldwide. BioPharma has clinical facilities both in the USA and Canada with a total capacity of 300 beds with access to healthy volunteers and special populations. Headquartered in Toronto, Canada, BioPharma’s comprehensive services also include Bioanalysis at our GLP Certified Laboratory, Scientific and Regulatory Affairs, Biostatistics and Safety Data Analysis (CDISC), Data Management and Medical Writing.
Popular Posts
-
What are early phase clinical trials?
Clinical Trials are divided into 4 phases. Phase 1 and 2 trials constitute early phase trials, Phase 3 and 4 research studies are late-phase trials.
The primary objective of Phase 1 studies is to determine the correct drug dosage by evaluating drug safety and determining if there are any side effects. Phase 1 trials are conducted in healthy volunteers.
Phase 2 studies also study the safety of a drug but focus on evaluating its effectiveness. These studies can be conducted in healthy volunteers or in individuals who have a certain disease or condition.
-
What is a clinical trial?
A Clinical trial is a process which is performed to determine whether an investigational drug, device or therapy is safe and effective. In early phase research (i.e. Phases 1 and 2), the safety and effectiveness of the drug will be evaluated in healthy volunteers.
-
What is an investigational drug?
An investigational drug can also be called an experimental drug and is being studied to see if your disease or medical condition improves while taking it. Scientists are trying to prove in clinical trials:
- If the drug is safe and effective.
- How the drug might be used in that disease.
- How much of the drug is needed.
- Information about the potential benefits and risks of taking the drug.
-
Why do you need to take blood draws and how many blood draws will be required?
In order to evaluate the drug profile, we need to understand its pharmacokinetics. This is essentially how the body reacts to a drug after its administration through the mechanisms of absorption, distribution, as well as the metabolic changes. Therefore, blood draws are collected at various time points to better understand this mechanism. Each study requires a specific number of blood draws and total blood volume. These values will be provided to you and clearly stipulated in the informed consent form (ICF). The amount of blood that will be taken is outlined in the ICF.
-
Should I expect to experience any side-effects while doing studies?
As every study is testing an investigational product, there may be side effects. You will be provided with a list of side effects that have been reported in previous trials (if any), so you can make an informed decision whether or not to participate in the trial. During the trial you will be required to immediately inform clinic study staff of any adverse effects that you are experiencing. These side effects usually resolve upon discontinuation of the study drug.
-
Will I be compensated for doing a clinical study?
Volunteers are compensated and the amount varies depending on the length of the clinical trial, length of stay and number of follow-up visits. The compensation is not specifically related to the risks or type of drug involved in the trials or studies. Every study is different and therefore, the compensation will vary. Study volunteers may receive between $1000 to $4000 for a trial (based on the factors listed above).
-
Are food and accommodation provided over the course of the trial?
Food – Clinical trials are conducted in a controlled setting which means that all food is provided and trial volunteers receive standardised meals. Individual meal plans or meal preferences cannot be provided. If you have any food allergies or hypersensitivity to food product(s) that are clinically significant or life-threatening you may not be able to participate in a trial. Please contact us to discuss any food issues.
Accommodation – During your in-clinic stay you will share sleeping areas with other volunteers who are of the same gender. Similar to a hospital setting, supervision will be provided to ensure that your health and safety are being monitored.
-
What is the length of a study and do I have to complete all the visits?
Details of the duration of a study can be found on the Volunteer Hub.
-
What is informed consent and how is it carried out?
Before you decide whether or not to take part in a clinical research study, you will be required to read and understand the information provided in an Informed Consent Form (ICF). The ICF describes the clinical research study and the nature of the investigational product to be used, including:
- Your rights and responsibilities as a study participant.
- What you will be asked to do during study participation.
- The potential risks that you should be aware of.
During this process, you will have the opportunity to discuss and ask questions related to the conduct of the clinical research study with the study doctor/ study staff. You are under no obligation to participate and your decision to take part in a clinical trial is voluntary.
-
Can I bring my own device?
Yes, we encourage you to bring items that will help to pass the time while you are in the clinic. You can use the time to study or work or catch up on the movies you’ve been meaning to watch.
-
What do I need to pack?
Wondering what to pack before your site visit? Visit our Packing List page to learn more.
-
When do I receive compensation for taking part in a study?
You will receive compensation as outlined during the Informed Consent process. Typically, you will receive compensation once all study visits have been completed. If, for any reason, you do not complete all study visits, your compensation will be on a pro-rated basis (i.e. for the time that you have participated in the trial)
-
Where will I sleep during the clinical study?
We provide a clean, safe socially distance sleeping environment, in a dormitory of hotel room style. Watch video
-
Can I bring my own food?
All aspects of clinical trials are closely monitored including the food and drink consumed by participants. While you are in the clinic, you will be provided with all meals as per the study guidelines. You will need to eat all the food provided to ensure the guidelines are met. Watch video
-
Privacy
We respect and value the privacy of our volunteers. View our Privacy and Cookie Policy here.



