Evaluation of Physical Dependence of CNS Drugs

Background on CNS Drugs
Companies regularly approach BioPharma Services to receive practical and pragmatic feedback on the FDA mandated physical dependence studies. Central nervous system or CNS drugs need to be assessed for abuse potential – determining if patients or the population at large may be interested in taking approved drugs for their rewarding property – the potential to be used as recreational drugs. In addition, there is a concern that with chronic use of a CNS drug that patients may face withdrawal symptoms with abrupt discontinuation, which may be indicative of physical dependence. Although the FDA guidelines on the assessment and phase 1 clinical trial design of abuse potential studies are relatively well-defined, withdrawal studies bring distinct issues that are characterized by the pharmacology of the CNS drug, the indication being treated, and the population that will use the medicine.
Although abuse potential and withdrawal information are required by various regulatory agencies, usually based on preclinical studies, the FDA has the most stringent and well-defined expectations that include clinical studies. The FDA has published various guidance that help sponsors determine the abuse potential of new chemical entities[i], but also to assess abuse deterrent formulations of CNS drugs known to be abused (e.g. opioids)[ii]. Finally, they also have been published a guidance for generic abuse deterrent formulations.[iii]
For new chemical entities, the FDA defines the requirements for physical dependence studies in the 2017 Guidance “Assessment of Abuse Potential of Drugs”.[i] Section E. “Clinical Evaluation of Physical Dependence” notes that an abuse potential assessment should include an evaluation of whether a CNS drug produces physical dependence. The purpose for this is two-fold. It is to provide accurate information in the product label for the healthcare provider and patient. This information is reported in Section 9 “Drug Abuse and Dependence” of a US approved label.
A secondary purpose of performing this assessment is to allow the FDA to determine if the CNS drug should be scheduled and what schedule the FDA will recommend. Note that some drugs (e.g. beta blockers and monoamine reuptake inhibitors) produce withdrawal symptoms but are not indicative that the drug has abuse potential and so may not need to be scheduled.
CNS Product Study Assessment
Unlike the human abuse potential study (HAP) the FDA does not necessarily require a separate study to assess physical dependence. In fact, determining the withdrawal symptoms as part of the Phase 3 studies is likely most appropriate in most cases. In this case, the CNS drug is given chronically to patients to assess the efficacy of the drug. At the end of the study, patients may stop taking the CNS drug abruptly as part of the study design, and this can be the logical time to assess withdrawal. It may be unethical to give the medication to healthy normal volunteers, especially chronically, if there are adverse events that are not an acceptable risk (e.g. as seen with some schizophrenia drugs).
On the other hand, stopping treatment in patients may also not be appropriate or ethical. For example, the abrupt discontinuation of CNS drugs for the treatment of epilepsy may result in seizures. The FDA prefers abrupt discontinuation to mimic the natural situation, rather than tapered discontinuation or precipitated withdrawal with an antagonist. In certain scenarios, the FDA will recommend a separately designed Phase 1 clinical study in healthy normal volunteers. This study would be a parallel study design with a placebo control.
In extreme cases, the FDA may accept or recommend appropriately designed animal studies if performing the study in a patient or volunteer population is not ethical due to the CNS drug’s safety profile or the inability to abruptly stop the drug. At the End of Phase 2 meeting, sponsors can propose this option.
CNS Product Withdrawal Symptoms Indicative of Physical Dependence
Symptoms of withdrawal symptoms indicative of physical dependence can include headache, anxiety, nausea/vomiting, tremor, chills, decreased concentration, agitation, irritability, sleep disturbance, mood changes and cognitive impairment. They may be opposite of the effects of the CNS drug – for example, opioids may cause constipation and withdrawal that can lead to diarrhea. A withdrawal study generally has patients or healthy normal volunteers take a drug chronically – long enough to reasonably have a chance to produce physical dependence – and the drug is then abruptly stopped. The study participants are then observed to see if they produce adverse events that are indicative of withdrawal. In addition, specific withdrawal scales and assessments should be done that are believed to be sensitive to the drug class and mechanism of action.
For example, for CNS drugs that have opioid-like properties, it may be appropriate to use the Clinical Opiate Withdrawal Scale (COWS) or the Subjective Opiate Withdrawal Scale (SOWS). For CNS drugs that are believed to have sedative effects, there are benzodiazepine type of scales that are sensitive to that type of withdrawal (e.g. Clinical Institute Withdrawal Assessment Scale for Benzodiazepines). Cognitive testing may also help to define the withdrawal symptoms.
Assessment of the Physical Dependence
The sponsor should characterize the drug with preclinical studies and in the phase 1 and 2 studies to determine the appropriate type of scales and measures to apply. Adverse events observed during the clinical studies may provide the sponsor some sense of withdrawal symptoms that subjects experience. During the End of Phase 2 FDA meeting and with input from the Controlled Substance Staff (CSS) the sponsor can propose and discuss the need and strategy for assessing the physical dependence for the drug.
The following evaluation may be included to assess physical dependence:[i]
- Use of drug class-specific withdrawal scales
- Use of disease-specific scales for evaluation of potential symptom rebound
- Assessment of AEs before and after drug discontinuation
- Use of VAS assessing withdrawal symptoms and mood states
- Use of daily diary by study subject
- Collection of physiological measures and vital signs
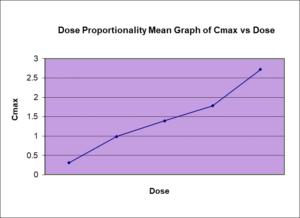
- Blood sampling for association of pharmacokinetics and withdrawal signs/symptoms
The Choice of Withdrawal Scale
The choice of withdrawal scale can be complicated by the intended effect of the drug. For example, a CNS drug being assessed for depression may lead to depression symptoms not as a result of withdrawal but related to lack of efficacy with discontinuation of the drug. This may be a situation that assessing in healthy, normal volunteers without symptoms of depression is warranted. The FDA recommends the use of disease specific scales to assess the potential symptom rebound.
It may be worthwhile to incorporate withdrawal assessments during the phase 2 studies. This can be helpful, in a smaller population, to see if certain withdrawal symptoms are observed. More scales could be applied. This information can then be used to inform the withdrawal component of a Phase 3 study.
The pharmacology of CNS drugs will impact the design of the study. For example, the half-life of the CNS drug will determine the monitored discontinuation period. The FDA requires that the observation period should be at least 5 half-lives to ensure that the drug is cleared. Although for short half-life drugs the observation period is short, the chance that the CNS drug produces withdrawal is higher as the drug no longer hits the target and the body has little time to adapt to the absence of the drug. Drugs with long half-life (or the active metabolite) means that the observation periods could take many days or even weeks.
Why Choose BioPharma Services?
The sponsor should make a careful assessment of the preclinical program and the Phase 1 and 2 results. This should inform the appropriate design that can be presented to the FDA at the end of Phase 2 study. Depending on the drug’s properties, the study may be done in patients as part of the Phase 3 study, done in HNV in a Phase 1 dependency study or in a non-clinical study. Not all labels have physical dependence information reported in their label (e.g. Finetepla and Potiga). That may be based on the nature of the drug or indication being treated. Even if not intending to provide information in the label, the FDA may still want to have this information for its scheduling. It is best to determine the strategy and then discuss this with the FDA.
Find out why BioPharma might be the right partner for you! Learn more about BioPharma Services and the wide array of services we provide.
BioPharma Services, Inc., a Think Research Corporation and clinical trial services company, is a full-service Contract Clinical Research Organization (CRO) based in Toronto, Canada, specializing in Phase 1 clinical trials 1/2a and Bioequivalence clinical trials for international pharmaceutical companies worldwide. BioPharma has clinical facilities both in the USA and Canada with access to healthy volunteers and special populations.